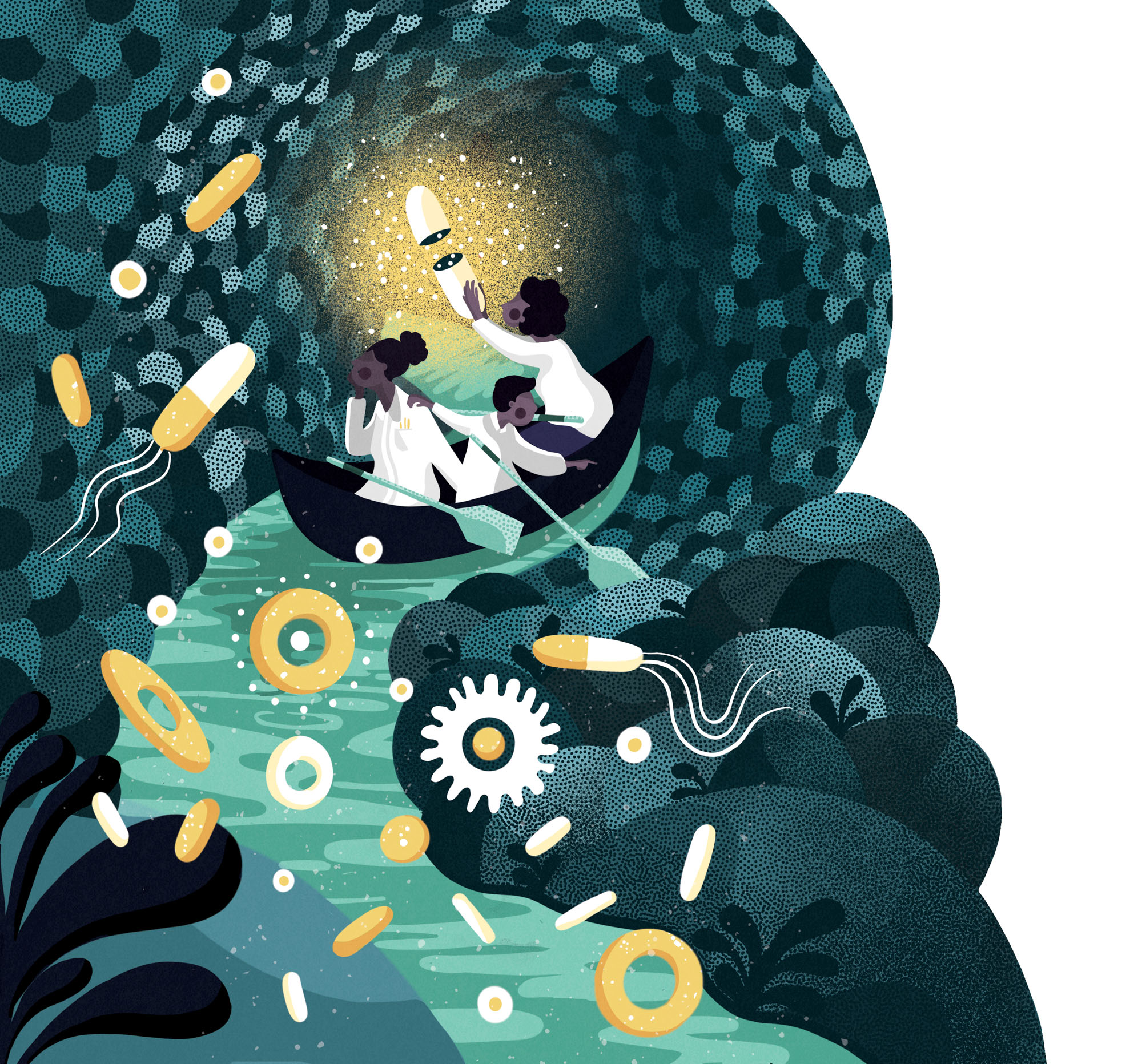
Let’s start with some imagination, make like a bacterium, and go inside your body. Maybe we’ll start by crawling around on your skin, then enter through one of the more germy, grimy portals, like the nose or the mouth. From there, we’ll slide down your throat and into your stomach. We might hang out here for a bit, seeing the sights, taking our time before we continue on through your intestines. Along the way to the inglorious exit, we’ll encounter all your body’s other friendly and unfriendly inhabitants. Which ones are the most helpful to you, and which ones could be dangerous? Could they be persuaded to work in your favor?
Our understanding of the tiny organisms living in and on us — the science of the microbiome — has been making massive strides. As we understand the full extent of their influence on our health and well-being, we are starting to devise new ways to work with them. It turns out we may be able to do a lot more than just live with our body’s microdenizens. Given the right training, they could be the key to curing a litany of complicated health problems.
And so, we return to your body, as an engineered microbe, a living medicine. This time, instead of passively traveling from entrance to exit, we have a mission. We can sense where to go, react to any changes in our environment, and hone in on the potential crisis area, such as a protein linked to cancer. This targeted, adaptable nature is the essential promise of using living organisms to treat challenging conditions like tumors or metabolic diseases. They have the potential to drastically change how we think about medicine.
Boosting Nature
When people think of medicine, they often perceive a dichotomy between pharmaceutical drugs and natural treatments. A preference for one side can even become an identity; on one extreme, you’ll find people who pop a pill for every ache or pain, and on the other, you’ll find those who will only try treatments derived from herbs or roots. But most people’s habits fall somewhere in between. And indeed, this reflects the way these two categories overlap in the real world. Just as aspirin got its name and healing powers from the healing shrub Spirea ulmaria, many pharmaceutical solutions are derived from plants and natural healing methods. Conversely, human engineering makes it much easier to administer natural treatments, as many supplemental medicines are extracted and processed in a lab.
Synthetic biology muddles this perceived distinction even more, drawing on the natural world to create custom lab-designed treatments. It combines biology and engineering to alter elements of the natural world for the benefit of human health outcomes. By editing bacteria, cells, and even fungi, it creates “living medicines” — organisms that react to conditions in the body to treat disease.
It’s helpful to think of this as an evolution of older techniques for augmenting our bodies and treating disease with living organisms — transplants and vaccines. An organ transplant places a new living system inside the body. A fecal transplant can introduce a living ecosystem of microbes into the gut, displacing a Clostridium difficile infection and restoring a healthy balance of bacteria. Vaccines unleash attenuated viruses into the body to train the immune system to fight pathogens. Engineered microbes are the next step in this modification of living things, whether they are gut bacteria replacing missing metabolic pathways or immune cells engineered with new cancer-targeting functions.
Training the Body
While vaccines train the immune system indirectly, living medicines are intended to directly engineer it. This shift can be seen in a new technique for treating cancer using the chimeric antigen receptor T-cells in the body, or CAR T-cells. One of the main players in the body’s immune system response, these cells seek out the specific proteins on pathogens, and destroy them. In CAR T-cell therapy, a cancer patient’s blood (or sometimes, a donor patient’s blood) is mined for these special cells. They are then taken out of the body, engineered to detect a protein specific to cancer cells, and eventually returned to the patient’s body to seek and destroy the malignancy. This treatment has already been FDA-approved for use in two types of cancers — specifically adult B-cell non-Hodgkin’s lymphoma and childhood acute lymphoblastic leukemia — and approval for more is soon to follow.
As we learn more about the relationship between the gut microbiome and bodily health, between the metabolism and brain, we are discovering new tasks for these engineered microbes.
CAR T-cell therapy could prove useful for other diseases too, as it can boost the immune system response without some of the limitations of a vaccine. Vaccines are not very effective if a patient is sick, as a weakened immune system can be resistant to training. CAR T-cell therapy can supplement the body’s immune system, offering a new way around this impasse.
Following a similar method and logic, engineered bacteria can be used to treat metabolic diseases. You might think of it as an evolution of probiotics, the “good” bacteria, like the Lactobacillus strains often found in yogurt. Synthetic biology can transform generically “good bacteria” into programmable, targeted disease fighters.
Synlogic, a Cambridge-based biotech company, is currently testing bacteria that treat phenylketonuria (PKU) in clinical trials, a rare metabolic disorder. People with this disease lack the enzyme to break down the amino acid phenylalanine, and so have to limit the protein in their diets or risk serious health problems. Synlogic has engineered a bacteria that breaks up the amino acid, allowing patients to eat as they please and live without that constant worry.
A vast assortment of diseases could be targeted with a focus on the gut. As we learn more about the relationship between the gut microbiome and bodily health, between the metabolism and brain, we are discovering new tasks for these engineered microbes.
Tending the Garden
While the main advantage of living drugs is that they are alive and adaptable, the flip side is that they could become harder to control. Anyone who has tended a garden knows that it can be challenging to achieve a balance between plants you want growing and plants that you don’t want growing. In the same way that weeds can take over, or that desired plants can dominate a garden, these new living treatments could choke out other strains in the microbiome. It is pivotal to design these bacteria so they don’t settle permanently in the body, lest they colonize it or transfer altered genes to other bacteria in the gut.
That’s not to mention the potential cost of such therapies. As specialized treatments, tailor-made to the patient, scaling the cost of production is sure to be an issue. A research article about CAR T-cell therapy outlined the prohibitive cost of the treatment, particularly if it turns out to be unsuccessful. “Although cancer persisted or recurred in three of five patients,” they write, “in practice, all patients will be charged the $373,000 price tag for the drug.” This may change if the treatments can be engineered to work on a wider scale for a more generalized group of people. But as long as they have to be individualized, the cost will continue to stick out even in a drastically overpriced healthcare system.
In short, living medicines carry many of the same risks as any other new medical inventions, including potential side effects and high costs, but the reward is immeasurably high. The fact that CAR-T therapy has proven effective at fighting specific cancers gives reason to hope that it could be applied to other cancers and immune disorders. This may be the next frontier in our path to self-discovery, in the most literal sense.